Effects of Healthcare System Design Problems
A bad system will beat a good person every time. W. Edwards Deming
Alongside impressive advances in technology, medication, equipment and knowledge over the last few decades, one aspect of healthcare has been overlooked – the human experience. Overlooking the human experience parallels a rise in dissatisfaction with healthcare, and a high rate of healthcare worker burnout. Dissatisfaction and burnout are effects of healthcare system design problems.
This is a serious problem.
Over half of Australian and US clinicians are experiencing symptoms of burnout – up to two times that of the general population, and up to three times the rate for other professionals. Burnout means that 32% of nurses in Australia are considering leaving the profession, at a time when the shortfall of nurses is increasing.
These burnout figures are pre-COVID, which has worsened the issue. If burnout was an infection, there would be a worldwide response similar to the COVID-epidemic response.
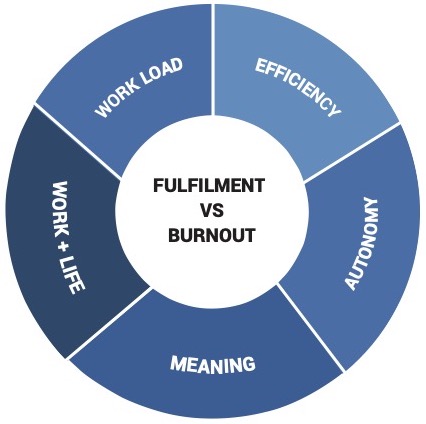
The primary drivers of burnout among clinicians are:
- Workload,
- Efficiency,
- Autonomy in work,
- Work-life integration, and
- Meaning in work.
Workload is poorly related to volume of work – it depends on factors such as location, workplace design and ergonomics; speciality and team structure, compensation arrangements, personal financial pressures, and compliance requirements. User surveys consistently report frustration in healthcare due to duplication of tasks, and manual cross-checking. These tasks are ideally suited to information technology, to free up humans from drudgery.
Efficiency is affected by training and experience, processes, team composition, integration of care and compliance requirements. Integration of care, and compliance checking/recording, are ideally suited to information technology – to free up humans from drudgery.
Autonomy varies with personality, control of scheduling, care guidelines, referral patterns and reimbursement restrictions. Scheduling, care guidelines and reimbursement criteria are ideally suited to information technology, to free up humans from drudgery.
The complexity of healthcare delivery, the enormous variation in size of facilities and the wide mix of operations that they perform means that a ‘one size fits all’ approach to improving user experience, healthcare quality and efficiency of delivery is destined to fail.
How do we tackle complexity?
An approach is required that minimises overlooking the essential elements, while allowing a degree of freedom for adaptation at the local level. This means considering:
- the requirements of healthcare providers,
- the needs of patients, and
- how to enable the supporting role of management and administrative personnel to both groups.
Analysing problems from the perspective of patients, healthcare providers and administrators potentially makes a requirements list very long. Finding common ground among these requirement becomes the essential ingredient to clarify the analysis and to formulate solutions. Supporting humans with these essential elements is ideally suited to information technology – to free up humans from drudgery.
What does this mean?
For example, individuals in separate functional areas often unintentionally duplicate problem-solving efforts, on behalf of their patients or downstream staff. Awareness of the shared effort in duplication is the beginnings of shared purpose. Identifying a simplified workflow that reduces exertion for the participants provides early rewards. Rewards encourage buy-in to the process.
Successful healthcare IT projects look for overlap and commonalities where IT can connect the dots and bridge the gaps. I’m always on the lookout for such providers, especially if they’ve been created to solve inefficiencies in the Australian context. Some providers that I work with are listed below.
If you know of any companies improving the user experience alongside efficiency and quality, please reach out!
– Read more at /book/
– Get in touch at /contact/
Excerpt From Reimagining Healthcare by A/Prof. Douglas Fahlbusch, MBBS, FANZCA, GAICD, GDM
(c) Perioperative Solutions Pty Ltd 2022
Paid Advisor to Surgical Order (SOx).
- Streamline Hospital Operations: efficient, risk-free theatre scheduling – simplify the logistics of planning and delivering a theatre list.
- Manage Inventory & Orders: Save time and money by managing stock with real-time updates for order status, billable items and expiring stock.
- Connect Practices, Hospitals and Suppliers: Surgeons’ Lists, Orders, and Preferences are all simplified and synchronised directly with Hospitals & Suppliers.

Advisor to Atidia.
Optimising patient care to improve patient outcomes and reduce costs, with:
- Digital Questionnaires: Conveniently and quickly gather essential background information from patients directly using a dynamic, multi-language, mobile-friendly app.
- Essential Risk Models: Automatically calculate baseline risk analyses such as BMI and ASA score. High risk conditions and medication issues are flagged.
- Smart protocols & safety: Automatically suggest patient, medication and test advice based on institution and best practice protocols. Make preoperative advice easy, repeatable and consistent.
- Anaesthetic Summary: Beautifully presented clinically relevant information, allowing for actionable insights, life-saving preparation and interventions.
- Quick & Easy Integration: Standalone or light integration with a range of EHR systems, either on-premise or in-cloud.
(commission-based)

Pro-bono Advisory Work:
Calvary Adelaide Hospital: technical and workflow advice to
- Medical Advisory Committee (MAC)
- Medication Safety Committee
- Perioperative Working Group
 Memorial Hospital: technical and workflow advice to the Paediatric Committee
Memorial Hospital: technical and workflow advice to the Paediatric Committee