How can we harness data to provide better healthcare?
We are overwhelmed with healthcare data. While we have a national e-health record, it doesn’t attempt to harness information from personal fitness devices and apps, our genome or siloed data in medical, nursing or allied health systems. Is the volume, not to mention the speed at which it is created, now part of the problem?
In a September 2022 Harvard Business Review article, Glaser et al examined the steps that are required to put data to work.
1. Measure Quality.
- Are we doing the right things?
- Are we getting the desired outcomes?
- What needs to change?
These are hard questions to answer. The Australian Commission on Safety and Quality in Healthcare, and its counterparts in other countries, seek to measure key outcome indicators, explore reasons for under-performance and create pathways for improvement.
Capacity.
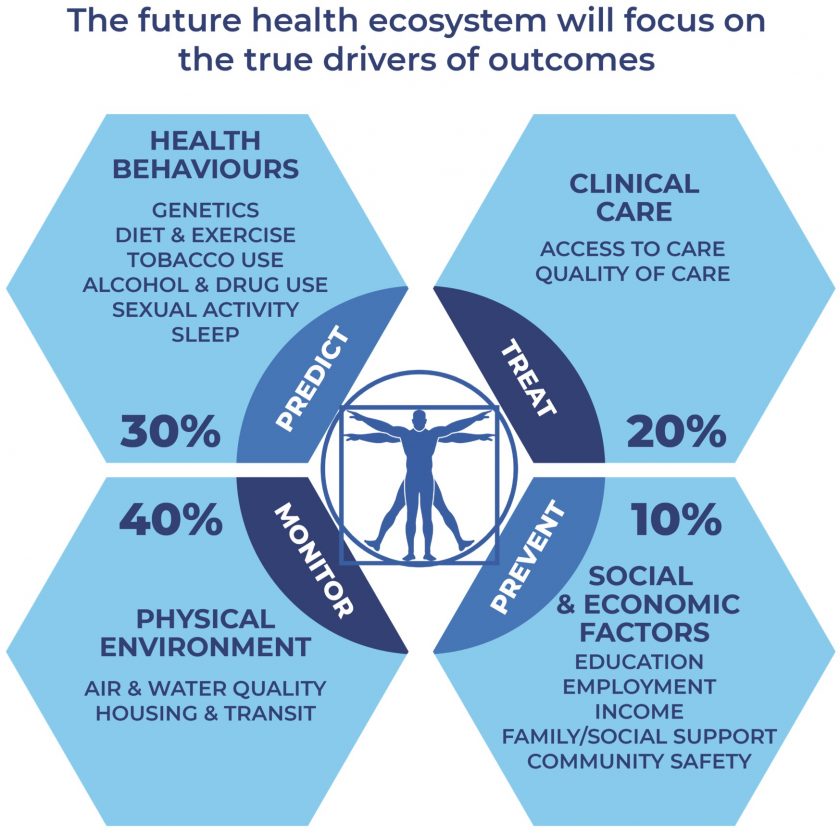
Increasing capacity by spending more money is often not the solution when we do not get the desired outcomes. More often, we are not doing the right things. Healthcare is not a production line – and people are not units of production. The determinants of health are primarily environmental and behavioural (see diagram), rather than the healthcare system itself. Our focus needs to include these extra inputs, although this increases the volume and velocity of data!
The inputs missing from healthcare
In addition, business processes affect clinical processes. For example, remuneration can have consequences on quality, availability and affordability of care. Money creates a moral hazard for organisations and individuals. It can create behaviours that:
- Favour highly paid interventions over lesser paid ones; or
- Pursue efficiency over quality service. Note that efficiency is good to a point to maximise the services delivered for a given healthcare spend, however this becomes a negative when profit alone is the outcome sought.
Funding.
Money can also create a ‘wrong pockets’ problem where:
- One organisation or individual bears the cost of an intervention and another benefits from the fix, creating a disincentive to a needed change; or
- Individuals benefit from ‘working slow’ to receive the same remuneration, leaving the organisation to bear the increased overheads for a fixed or decreasing income.
Compliance.
Governance and regulation are blunt instruments to tackle these issues. Team and individual feedback is essential for locally relevant innovation and improvement. Remuneration based on outcomes such as quality, availability, affordability and personalisation, and not just volume, helps to support innovation and improvement.
2. Claims Data
Claims Data is a business process that could be used for clinical improvement. While core to business practices, these data are incomplete for clinical purposes. Claims data tell us what was done, however do not track or report outcomes. And claims data tend to be weeks or months old by the time that they are compiled. Modern data systems can support real-time reporting, and linkage for population and individual health improvement. We just need to design the systems to achieve these outcomes.
3. Digital Measures and Monitoring
As previously mentioned, the national e-health record doesn’t attempt to harness information from personal fitness devices and apps, our genome or siioed data in medical, nursing or allied health systems. Combining these data to Quality and Claims data will enable improvements in both population and individual healthcare. Machine learning can amplify the ability of humans to make sense of the volume and speed of data being created, to identify patterns both positive and negative.
4. Don’t reinvent the wheel.
Britnell ‘In Search of the Perfect Health System’ in 2015 analysed over 25 health systems from 60 globally to discover that no country does everything well. However, each country has a strength from which other countries can learn. Denmark and Estonia arguably are leading the way in digitisation. We can avoid any mis-steps that they, and others, may have made.
What should we do?
A To-Do list to harness data to improve healthcare.
- Reduce the cost of data collection, and improve its timeliness. These outcomes may appear to conflict, however this is the strength of digital. Apps and wearable can automatically upload data via networks – both cheap and fast. We need to design healthcare delivery systems so that they are able to automate the collection of data, improving its timeliness while reducing the cost. Paper-based, manual entry systems no longer have a place. Nor do time-consuming manual data-extraction techniques.
- Expand the range of collected data. Linking the social determinants of health (see figure) to healthcare outcomes will uncover new ways to improve the quality, accessibility and affordability of healthcare.
- Leverage clinical and business process healthcare data. Process automation, machine learning and ‘artificial intelligence’ can reduce the overhead in providing clinical care, and augment clinical decisions and actions. We need tools that facilitate collaboration among healthcare’s numerous stakeholders.
- Establish a digital foundation for the improvement of processes that gather, analyse and report data, quality and outcome measures. This will improve the transparency and usefulness of data and its linkages. One of our current difficulties is that funders, regulators and professional societies differ in their approaches and foci, resulting in considerable variations in care that do not add to the quality, affordability, accessibility or availability of healthcare.
What is the impact of digital healthcare measures?
- Clinicians can improve their clinical performance and cost-effectiveness.
- Patients can make more informed, inclusive choices that are tailored to the factors that matter to them.
- Payers can better serve their patients and healthcare providers with more cost-effective quality care.
In summary, applying the same data-driven processes to healthcare that are utilised by other industries such as financial services, retailing and social media will yield the same improvements in efficiency, personalisation and quality for the benefit of healthcare. Patients, providers and society all benefit.
Further Reading.
Britnell M. ‘In Search of the Perfect Health System’, Bloomsbury Academic 2015
Glaser J et al. How to Use Digital Health Data to Improve Outcomes. HBR Online 12SEP22